One of the great pleasures of my job is getting to meet the high school students who take part in our SPARK or Summer Internship to Accelerate Regenerative Medicine Knowledge program. It’s a summer internship for high school students where they get to spend a couple of months working in a world class stem cell and gene therapy research facility. The students, many of whom go into the program knowing very little about stem cells, blossom and produce work that is quite extraordinary.
One such student is Tan Ieng Huang, who came to the US from China for high school. During her internship at U.C. San Francisco she got to work in the lab of Dr. Arnold Kriegstein. He is the Founding Director of the Eli and Edythe Broad Center of Regeneration Medicine and Stem Cell Research at the University of California, San Francisco. Not only did she work in his lab, she took the time to do an interview with him about his work and his thoughts on the field.
It’s a fascinating interview and shows the creativity of our SPARK students. You will be seeing many other examples of that creativity in the coming weeks. But for now, enjoy the interview with someone who is a huge presence in the field today, by someone who may well be a huge presence in the not too distant future.
‘a tête-à-tête with Prof. Arnold Kriegstein’

Prof. Arnold Kriegstein is the Founding Director of the Eli and Edythe Broad Center of Regeneration Medicine and Stem Cell Research at the University of California, San Francisco. Prof. Kriegstein is also the Co-Founder and Scientific Advisor of Neurona Therapeutics which seeks to provide effective and safe cell therapies for chronic brain disorder. A Clinician by training, Prof. Kriegstein has been fascinated by the intricate workings of the human brain. His laboratory focuses on understanding the transcriptional and signaling networks active during brain development, the diversity of neuronal cell types, and their fate potential. For a long time, he has been interested in harnessing this potential for translational and therapeutic intervention.
During my SEP internship I had the opportunity to work in the Kriegstein lab. I was in complete awe. I am fascinated by the brain. During the course of two months, I interacted with Prof. Kriegstein regularly, in lab meetings and found his ideas deeply insightful. Here’s presenting some excerpts from some of our discussions, so that it reaches many more people seeking inspiration!
Tan Ieng Huang (TH): Can you share a little bit about your career journey as a scientist?
Prof. Arnold Kriegstein (AK): I wanted to be a doctor when I was very young, but in high school I started having some hands-on research experience. I just loved working in the lab. From then on, I was thinking of combining those interests and an MD/PhD turned out to be an ideal course for me. That was how I started, and then I became interested in the nervous system. Also, when I was in high school, I spent some time one summer at Rockefeller University working on a project that involved operant conditioning in rodents and I was fascinated by behavior and the role of the brain in learning and memory. That happened early on, and turned into an interest in cortical development and with time, that became my career.
TH: What was your inspiration growing up, what made you take up medicine as a career?
AK: That is a little hard to say, I have an identical twin brother. He and I used to always share activities, do things together. And early on we actually became eagle scouts, sort of a boy scout activity in a way. In order to become an eagle scout without having to go through prior steps, we applied to a special program that the scouts had, which allowed us to shadow physicians in a local hospital. I remember doing that at a very young age. It was a bit ironic, because one of the evenings, they showed us films of eye surgery, and my brother actually fainted when they made an incision in the eye. The reason it makes me laugh now is because my brother became an eye surgeon many years later. But I remember our early experience, we both became very fascinated by medicine and medical research.

TH: What inspired you to start the Eli and Edythe Broad Center of Regeneration Medicine and Stem Cell Research Institute?
AK: My interest in brain development over the years became focused on earlier stages of development and eventually Neurogenesis, you know, how neurons are actually generated during early stages of in utero brain development. In the course of doing that we discovered that the radial glial cells, which have been thought for decades to simply guide neurons as they migrate, turned out to actually be the neural stem cells, they were making the neurons and also guiding them toward the cortex. So, they were really these master cells that had huge importance and are now referred to as neural stem cells. But at that time, it was really before the stem cell field took off. But because we studied neurogenesis, because I made some contributions to understanding how the brain develops from those precursors or progenitor cells, when the field of stem cells developed, it was very simple for me to identify as someone who studied neural stem cells. I became a neural stem cell scientist. I started a neural stem cell program at Columbia University when I was a Professor there and raised 15 million dollars to seed the program and hired new scientists. It was shortly after that I was approached to join UCSF as the founder of a new stem cell program. And it was much broader than the nervous system; it was a program that covered all the different tissues and organ systems.
TH: Can you tell us a little bit about how stem cell research is contributing to the treatment of diseases? How far along are we in terms of treatments?
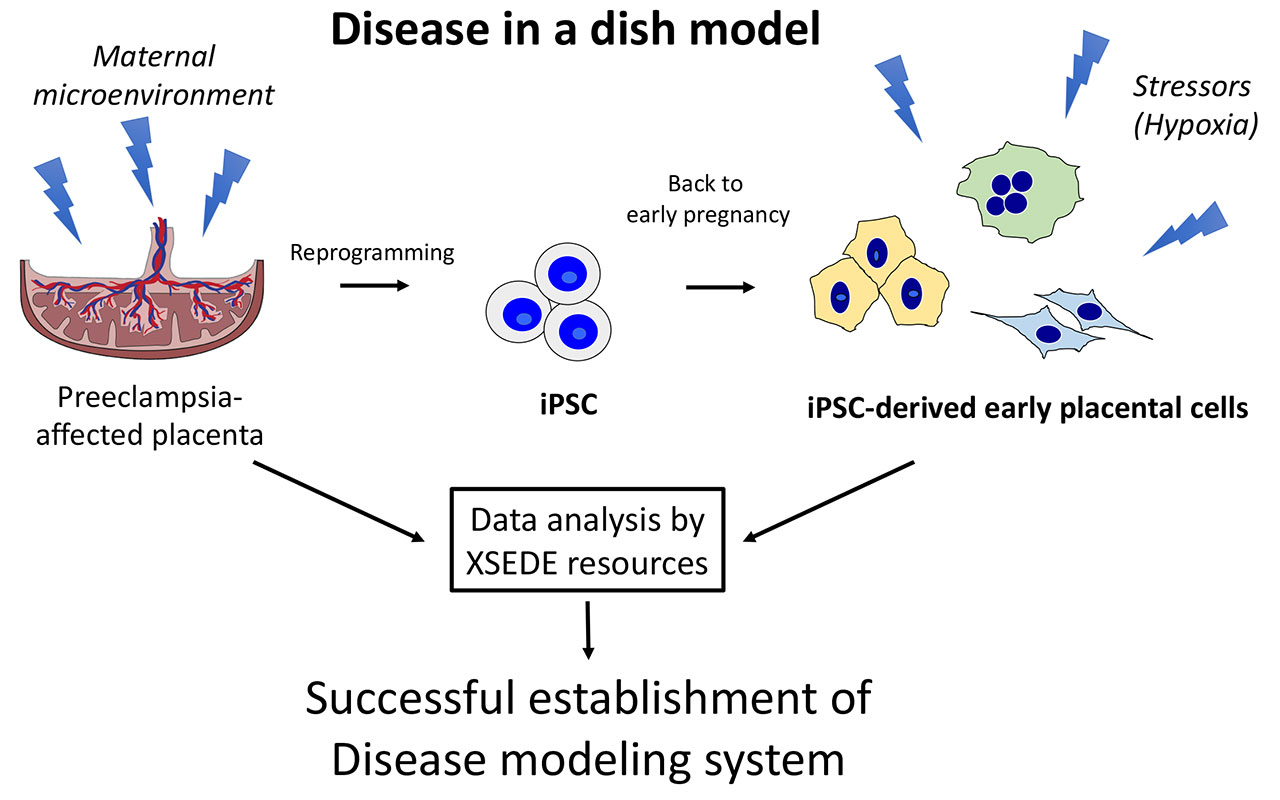
AK: It’s taken decades, but things are really starting to reach the clinic now. The original work was basic discovery done in research laboratories, now things are moving towards the clinic. It’s a really very exciting time. Initially the promise of stem cell science was called Regenerative medicine, the idea of replacing injured or worn-out tissues or structures with new cells and new tissues, new organs, the form of regeneration was made possible by understanding that there are stem cells that can be tweaked to actually help make new cells and tissues. Very exciting process, but in fact the main progress so far hasn’t been replacing worn out tissues and injured cells, but rather understanding diseases using human based model of disease. That’s largely because of the advent of induced pluripotent stem cells, a way of using stem cells to make neurons or heart cells or liver cells in the laboratory, and study them both in normal conditions during development and in disease states. Those platforms which are relatively easy to make now and are pretty common all over the world allow us to study human cells rather than animal cells, and the hope is that by doing that we will be able to produce conventional drugs and treatments that work much better than ones we had in the past, because they will be tested in actual human cells rather than animal cells.
TH: That is a great progress and we have started using human models because even though there are similarities with animal models, there are still many species-specific differences, right?
AK: Absolutely, in fact, one of the big problems now in Big Pharma, you know the drug companies, is that they invest millions and sometimes hundreds of millions of dollars in research programs that are based on successes in treating mice, but patients don’t respond the same way. So the hope is that by starting with a treatment that works on human cells it might be more likely that the treatment will work on human patients.
TH: What are your thoughts on the current challenges and future of stem cell research?
AK: I think this is an absolute revolution in modern medicine, the advent of two things that are happening right now, first the use of induced pluripotent stem cells, the ability to make pluripotent cells from adult tissue or cells from an individual allows us to use models of diseases that I mentioned earlier from actual patients. That’s one major advance. And the other is gene editing, and the combination of gene editing and cell-based discovery science allows us to think of engineering cells in ways that can make them much more effective as a form of cell therapy and those cell therapies have enormous promise. Right now, they are being used to treat cancer, but in the future, they might be able to treat heart attack, dementia, neurodegenerative diseases, ALS, Parkinson’s disease, a huge list of disorders that are untreatable right now or incurable. They might be approached by the combination of cell-based models, cell therapies, and gene editing.
TH: I know there are still some challenges right now, like gene editing has some ethical issues because people don’t know if there can be side effects after the gene editing, what are your thoughts?
AK: You know, like many other technologies there are uncertainties, and there are some issues. Some of the problems are off-target effects, that is you try to make a change in one particular gene, and while doing that you might change other genes in unexpected ways and cause complications. But we are understanding that more and more now and can make much more precise gene editing changes in just individual genes without affecting unanticipated areas of the genome. And then there are also the problems of how to gene-edit cells in a safe way. There are certain viral factors that can be used to introduce the gene editing apparatus into a cell, and sometimes if you are doing that in a patient, you can also have unwanted side effects from the vectors that you are using, often they are modified viral vectors. So, things get complicated very quickly when you start trying to treat patients, but I think these are all tractable problems and I think in time they will all be solved. It will be a terrific, very promising future when it comes to treating patients who are currently untreatable.
TH: Do you have any advice for students who want to get into this field?
AK: Yes, I think it’s actually never been a better time and I am amazed by the technologies that are available now. Gene editing that I mentioned before but also single cell approaches, the use of single cell multiomics revealing gene expression in individual cells, the molecular understanding of how individual cells are formed, how they are shaped, how they change from one stage to another, how they can be forced into different fates. It allows you to envision true Regenerative medicine, improving health by healing or replacing injured or diseased tissues. I think this is becoming possible now, so it’s a very exciting time. Anyone who has an interest in stem cell biology or new ways of treating diseases, should think about getting into a laboratory or a clinical setting. I think this time is more exciting than it’s ever been.
TH: So excited to hear that, because in school we have limited access to the current knowledge, the state-of-art. I want to know what motivates you every day to do Research and contribute to this field?
AK: Well, you know that I have been an MD/PhD, as I mentioned before, in a way, there are two different reward systems at play. In terms of the PhD and the science, it’s the discovery part that is so exciting. Going in every day and thinking that you might learn something that no one has ever known before and have a new insight into a mechanism of how something happens, why it happens. Those kinds of new insights are terrifically satisfying, very exciting. On the MD side, the ability to help patients and improve peoples’ lives is a terrific motivator. I always wanted to do that, was very driven to become a Neurologist and treat both adult and pediatric patients with neurological problems. In the last decade or so, I’ve not been treating patients so much, and have focused on the lab, but we have been moving some of our discoveries from the laboratory into the clinic. We have just started a clinical trial, of a new cell-based therapy for epilepsy in Neurona Therapeutics, which is really exciting. I am hoping it will help the patients but it’s also a chance to actually see something that started out as a project in the laboratory become translated into a therapy for patients, so that’s an achievement that has really combined my two interests, basic science, and clinical medicine. It’s a little late in life but not too late, so I’m very excited about that.
Tan Ieng Huang, Kriegstein Lab, SEP Intern, CIRM Spark Program 2022