Two voices, one message, watch out for predatory stem cell clinics
Last week two new papers came out echoing each other about the dangers of bogus “therapies” being offered by predatory stem cell clinics and the risks they pose to patients.
The first was from the Pew Charitable Trusts entitled: ‘Harms Linked to Unapproved Stem Cell Interventions Highlight Need for Greater FDA Enforcement’ with a subtitle: ‘Unproven regenerative medical products have led to infections, disabilities, and deaths.’
That pretty much says everything you need to know about the report, and in pretty stark terms; need for greater FDA enforcement and infections, disabilities and deaths.
Just two days later, as if in response to the call for greater enforcement, the Food and Drug Administration (FDA) came out with its own paper titled: ‘Important Patient and Consumer Information About Regenerative Medicine Therapies.’ Like the Pew report the FDA’s paper highlighted the dangers of unproven and unapproved “therapies” saying it “has received reports of blindness, tumor formation, infections, and more… due to the use of these unapproved products.”
The FDA runs down a list of diseases and conditions that predatory clinics claim they can cure without any evidence that what they offer is even safe, let alone effective. It says Regenerative Medicine therapies have not been approved for the treatment of:
- Arthritis, osteoarthritis, rheumatism, hip pain, knee pain or shoulder pain.
- Blindness or vision loss, autism, chronic pain or fatigue.
- Neurological conditions like Alzheimer’s and Parkinson’s.
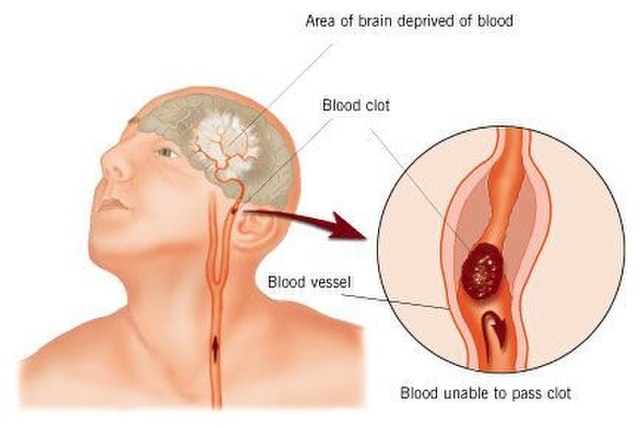
- Heart disease, lung disease or stroke.
The FDA says it has warned clinics offering these “therapies” to stop or face the risk of legal action, and it warns consumers: “Please know that if you are being charged for these products or offered these products outside of a clinical trial, you are likely being deceived and offered a product illegally.”
It tells consumers if you are offered one of these therapies – often at great personal cost running into the thousands, even tens of thousands of dollars – you should contact the FDA at ocod@fda.hhs.gov.
The Pew report highlights just how dangerous these “therapies” are for patients. They did a deep dive into health records and found that between 2004 and September 2020 there were more than 360 reported cases of patients experiencing serious side effects from a clinic that offered unproven and unapproved stem cell procedures.
Those side effects include 20 deaths as well as serious and even lifelong disabilities such as:
- Partial or complete blindness (9).
- Paraplegia (1).
- Pulmonary embolism (6).
- Heart attack (5).
- Tumors, lesions, or other growths (16).
- Organ damage or failure in several cases that resulted in death.
More than one hundred of the patients identified had to be hospitalized.
The most common type of procedures these patients were given were stem cells taken from their own body and then injected into their eye, spine, hip, shoulder, or knee. The second most common was stem cells from a donor that were then injected.
The Pew report cites the case of one California-based stem cell company that sold products manufactured without proper safety measures, “including a failure to properly screen for communicable diseases such as HIV and hepatitis B and C.” Those products led to at least 13 people being hospitalized due to serious bacterial infection in Texas, Arizona, Kansas, and Florida.
Shocking as these statistics are, the report says this is probably a gross under count of actual harm caused by the bogus clinics. It says the clinics themselves rarely report adverse events and many patients don’t report them either, unless they are so serious that they require medical intervention.
The Pew report concludes by saying the FDA needs more resources so it can more effectively act against these clinics and shut them down when necessary. It says the agency needs to encourage doctors and patients to report any unexpected side effects, saying: “devising effective strategies to collect more real-world evidence of harm can help the agency in its efforts to curb the growth of this unregulated market and ensure that the regenerative medicine field develops into one that clinicians and patients can trust and safely access.”
We completely support both reports and will continue to work with the FDA and anyone else opposed to these predatory clinics. You can read more here about what we have been doing to oppose these clinics, and here is information that will help inform your decision if you are thinking about taking part in a stem cell clinical trial but are not sure if it’s a legitimate one.