One of the reasons why it’s so hard to develop treatments for problems in the brain – things like Alzheimer’s, autism and schizophrenia – is that you can’t do an autopsy of a living brain to see what’s going wrong. People tend to object. To get around that, scientists have used stem cells to create models of what’s happening inside the brain. They’re good, but they have their limitations. Now a team at the Salk Institute for Biological Studies has found a way to create a better brain model, and hopefully a faster route to developing new treatments.
For a few years now, scientists have been able to take skin cells from patients with neurodegenerative disorders and turn them into neurons, the kind of brain cell affected by these different diseases. They grow these cells in the lab and turn them into clusters of cells, so-called brain “organoids”, to help us better understand what’s happening inside the brain and even allow us to test medications on them to see if those treatments can help ease some symptoms.
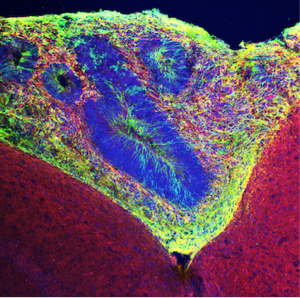
Human organoid tissue (green) grafted into mouse tissue. Neurons are labeled with red. Credit: Salk Institute
But those models don’t really capture the complexity of our brains – how could they – and so only offer a glimpse into what’s happening inside our skulls.
Now the team at Salk have developed a way of transplanting these organoids into mouse brains, giving them access to oxygen and nutrients that can help them not only survive longer but also display more of the characteristics found in the human brain.
In a news release, CIRM Grantee and professor at Salk’s Laboratory of Genetics, Rusty Gage said this new approach gives researchers a powerful new tool:
“This work brings us one step closer to a more faithful, functional representation of the human brain and could help us design better therapies for neurological and psychiatric diseases.”
The transplanted human brain organoids showed plenty of signs that they were becoming engrafted in the mouse brain:
- They had blood vessels form in them and blood flowing through them
- They formed neurons
- They formed other brain support cells called astrocytes
They also used a series of imaging techniques to confirm that the neurons in the organoid were not just connecting but also sending signals, in essence, communicating with each other.
Abed AlFattah Mansour, a Salk research associate and the paper’s first author, says this is a big accomplishment.
“We saw infiltration of blood vessels into the organoid and supplying it with blood, which was exciting because it’s perhaps the ticket for organoids’ long-term survival. This indicates that the increased blood supply not only helped the organoid to stay healthy longer, but also enabled it to achieve a level of neurological complexity that will help us better understand brain disease.”
A better understanding of what’s going wrong is a key step in being able to develop new treatments to fix the problem.
The study is published in the journal Nature Biotechnology.
CIRM has a double reason to celebrate this work. Not only is the team leader, Rusty Gage, a CIRM grantee but one of the Salk team, Sarah Fernandes, is a former intern in the CIRM Bridges to Stem Cell Research program.

From left: Sarah Fernandes, Daphne Quang, Stephen Johnston, Sarah Parylak, Rusty Gage, Abed AlFattah Mansour, Hao Li Credit: Salk Institute