The American Cancer Society estimates that this year in the United States, there will be 268,490 new cases of prostate cancer. It also estimates that 34,500 men will die from the cancer in 2022. Other than skin cancer, prostate cancer is the most common cancer in American men.
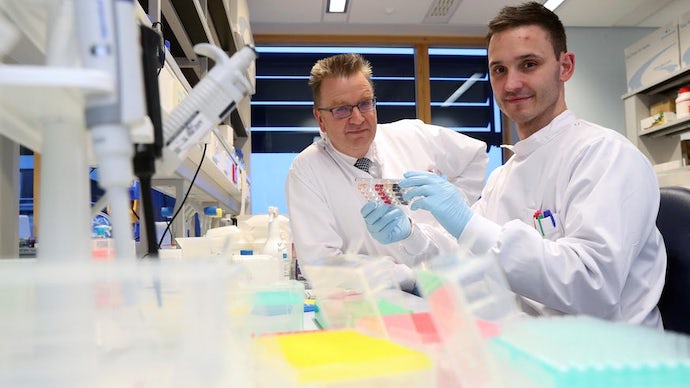
These stark statistics are why the California Institute for Regenerative Medicine (CIRM) has awarded a $5.8 million grant to researchers at the University of Southern California to begin conducting preclinical studies using an innovative treatment for prostate cancer, known as synthetic immune receptor (SIR-T) therapy.
“We have a homegrown USC technology which shows a lot of promise. If the path that we are on ultimately proves successful, it could revolutionize the treatment of not only prostate cancer but also other cancers,” said principal investigator Dr. Preet M. Chaudhary, a professor of medicine at the Keck School of Medicine of USC.
A new approach to immunotherapy
CAR-T cell therapy—which is now approved by the U.S. Food and Drug Administration (FDA) to treat several blood cancers—has been revolutionary for certain patients. In CAR-T therapy, a patient’s T-cells—a key part of their immune system—are extracted and genetically engineered to express the chimeric antigen receptor (CAR). The modified T-cells are then reinjected into the patient, where CAR enables them to selectively seek out, bind to, and kill cancer cells.
But its success in treating blood cancers has not translated into effectiveness against solid tumor cancers, such as prostate, breast, brain, gastrointestinal, skin and lung cancer.
“The bottom line is that people have tried to replicate the success of CAR-T cell therapy with solid tumor cancers, and have been mostly unsuccessful,” Chaudhary said.
SIR-T therapy, in contrast, uses different receptors that more closely resemble the body’s natural T-cells. Chaudhary and his team tested thousands of prototypes over an eight-year period to develop receptors that are effective and safe for solid tumors, including prostate cancer. An initial round of tests in mice yielded very promising results, prompting Chaudhary to apply for funding from CIRM.
What’s next?
With CIRM funding, Chaudhary and his team can now begin conducting preclinical trials of SIR-T therapy. Their research over the next two and a half years will culminate in an application for FDA approval to begin clinical trials in humans.
Chaudhary’s lab is also testing SIR-T therapy for other types of cancer, including melanoma, kidney cancer, lymphoma and a different molecule involved in prostate cancer.
“This technology has a lot of different applications, so we are working to ensure the platform works across disease types,” Chaudhary said. “The series of grants we’ve received reflects a lot of excitement about the SIR-T platform.”
To learn more about the work CIRM has funded to better understand solid tumors, visit our Solid Tumor Fact Sheet web page.