More often than not, people don’t really think about their blood sugar levels before sitting down to enjoy a delicious meal, partake in a tasty dessert, or go out for a bicycle ride. But for type 1 diabetes (T1D) patients, every minute and every action revolves around the readout from a glucose meter, a device used to measure blood sugar levels.
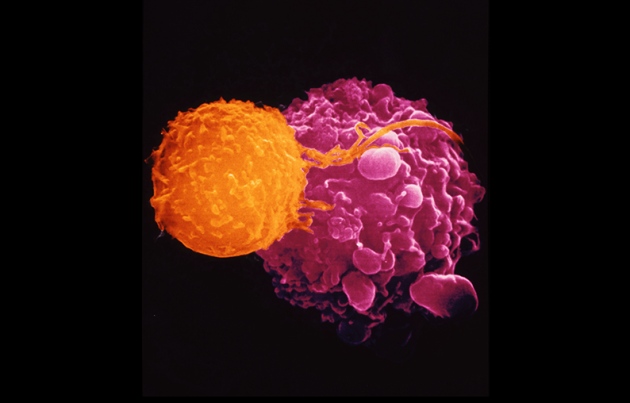
Normally, the pancreas contains beta cells that produce insulin in order to maintain blood sugar levels in the normal range. Unfortunately, those with T1D have an immune system that destroys their own beta cells, thereby decreasing or preventing the production of insulin and in turn the regulation of blood sugar levels. Chronic spikes in blood sugar levels can lead to blindness, nerve damage, kidney failure, heart disease, stroke, and even death.
Those with T1D manage their condition by injecting themselves with insulin anywhere from two to four times a day. A light workout, slight change in diet, or even an exciting event can have a serious impact that requires a glucose meter check and an insulin injection.
There are clinical trials involving transplants of pancreatic “islets”, clusters of cells containing healthy beta cells, but these rely on pancreases from deceased donors and taking immune suppressing drugs for life.
But what if there was a way to produce healthy beta cells in a lab without the need of a transplant?
Dr. Matthias Hebrok, director of the UCSF diabetes center, and Dr. Gopika Nair, postdoctoral fellow, have discovered how to transform human stem cells into healthy, insulin producing beta cells.
In a news release written by Dr. Nicholas Weiler of UCSF, Dr. Hebrok is quoted as saying “We can now generate insulin-producing cells that look and act a lot like the pancreatic beta cells you and I have in our bodies. This is a critical step towards our goal of creating cells that could be transplanted into patients with diabetes.”
For the longest time, scientists could only produce cells at an immature stage that were unable to respond to blood sugar levels and secrete insulin properly. Dr. Hebrok and Dr. Nair discovered that mimicking the “islet” formation of cells in the pancreas helped the cells mature. These cells were then transplanted into mice and found that they were fully functional, producing insulin and responding to changes blood sugar levels.
Dr. Hebrok’s team is already in collaboration with various colleagues to make these cells transplantable into patients.
Dr. Nair in the article is also quoted as saying “Current therapeutics like insulin injections only treat the symptoms of the disease. Our work points to several exciting avenues to finally finding a cure.”
“We’re finally able to move forward on a number of different fronts that were previously closed to us,” Hebrok added. “The possibilities seem endless.”
Dr. Hebrok, who is also a member of the CIRM funded UCSF Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research, was senior author of the new study, which was published February 1, 2019 in Nature Cell Biology.
CIRM has funded three separate human clinical trials for T1D that total approximately $37.8 million in awards. Two of these trials are being conducted by ViaCyte, Inc. and the third trial is being conducted by Caladrius Biosciences.