Today is an exciting day for diabetes research and patients. For the first time, scientists have succeeded in making functional pancreatic beta cells from human skin. This new method for making the insulin-producing cells of the pancreas could produce a new, more effective treatment for patients suffering from diabetes.
Researchers at the Gladstone Institutes and the University of California, San Francisco published these promising findings today in the journal Nature Communications.
Making pancreatic cells from skin
They used a technique called direct reprogramming to turn human skin cells directly into pancreatic beta cells without having to go all the way back to a pluripotent stem cell state. The skin cells were treated with factors used to generate induced pluripotent stem cells (iPSCs) and with pancreatic-specific molecules. This cocktail of factors and molecules shut off the skin genes and turned on genes of the pancreas.
The end product was endoderm progenitor cells, which are like stem cells but can only generate cell types specific to organs derived from the endoderm layer (for example: lungs, thyroid, pancreas). The scientists took these endoderm progenitors and further coaxed them into mature, pancreatic beta cells after treatment with another cocktail of molecules.
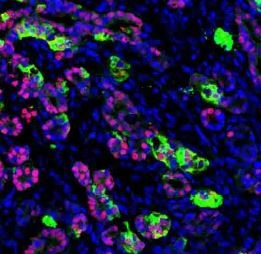
Functioning human pancreatic cells after they’ve been transplanted into a mouse. (Image: Saiyong Zhu, Gladstone)
While the pancreatic cells they made looked and acted like the real thing in a dish (they were able to secrete insulin when exposed to glucose), the authors needed to confirm that they functioned properly in animals. They transplanted the mature beta cells into mice that were engineered to have diabetes, and observed that the human beta cells protected the mice from becoming diabetic by properly regulating their blood glucose levels.
Importantly, none of the mice receiving human cells got tumors, which is always a concern when transplanting reprogrammed cells or cells derived from pluripotent stem cells.
What does this mean?
This study is groundbreaking because it offers a new and more efficient method to make functioning human beta cells in mass quantities.
Dr. Sheng Ding, a CIRM funded senior investigator at the Gladstone and co-senior author, explained in a Gladstone news release:
“This new cellular reprogramming and expansion paradigm is more sustainable and scalable than previous methods. Using this approach, cell production can be massively increased while maintaining quality control at multiple steps. This development ensures much greater regulation in the manufacturing process of new cells. Now we can generate virtually unlimited numbers of patient-matched insulin-producing pancreatic cells.”
Matthias Hebrok, director of the Diabetes Center at UCSF and co-senior author on paper discussed the potential research and clinical applications of their findings:
“Our results demonstrate for the first time that human adult skin cells can be used to efficiently and rapidly generate functional pancreatic cells that behave similar to human beta cells. This finding opens up the opportunity for the analysis of patient-specific pancreatic beta cell properties and the optimization of cell therapy approaches.”
The study does mention the caveat that their direct reprogramming approach wasn’t able to generate all the cell types of the pancreas. Having these support cells would better recreate the pancreatic environment and likely improve the function of the transplanted beta cells.
Lastly, I find this study exciting because it kills two birds with one stone. Scientists can use this technique to make better cellular models of diabetes to understand why the disease happens, and they could also develop new cell replacement therapies in humans. Already, stem cell derived pancreatic beta cells are being tested in human clinical trials for type 1 diabetes (one of them is a CIRM-funded clinical trial by Viacyte) and it seems likely that beta cells derived from skin will follow suit.
Related links:

