
Bottom Left to right: Elizabeth Crouch, PhD; Mohammed Mostajo-Radji, PhD; Carrie Beardon, PhD; Michael Zito, MD
As part of our goal of accelerating discoveries and therapies for central nervous system disorders, in 2023, the California Institute for Regenerative Medicine (CIRM) launched a program specifically funding research into neuro diseases called the Research using Multidisciplinary, Innovative approaches in Neuro Diseases (ReMIND) Program, it supported seven projects worth over $80 million. That program later became part of CIRM’s discovery stage funding programs and was renamed ReMIND-L (DISC4).
CIRM awarded Aparna Bhaduri, PhD, from UCLA awarded $10.3 million as part of the 2023 ReMIND program along with her co-investigators Heather Christofk, PhD, Harley Kornblum, PhD, and William Zeiger, MD, PhD, also from UCLA, and Elizabeth Crouch, PhD, from UCSF, and Mohammed Mostajo-Radji, PhD, of UCSC. Together, they are exploring early stages of brain development and how mutations linked to autism and schizophrenia alter the normal process.
CIRM connected with Dr. Bhaduri to learn more about the project and how it could eventually help detect and treat people with autism or schizophrenia.
Some responses have been edited for clarity and brevity:
CIRM: Please share a summary of your research project. Is there a particular disease focus? Is there a broader question that this project is hoping to address?
Dr. Bhaduri: Every child’s brain is fed by a bustling partnership between nerve cells and tiny blood vessels. We’re asking: how does the brain’s energy supply—its “metabolism”—guide that partnership, and what happens when the script is altered in neurodevelopmental disorders?
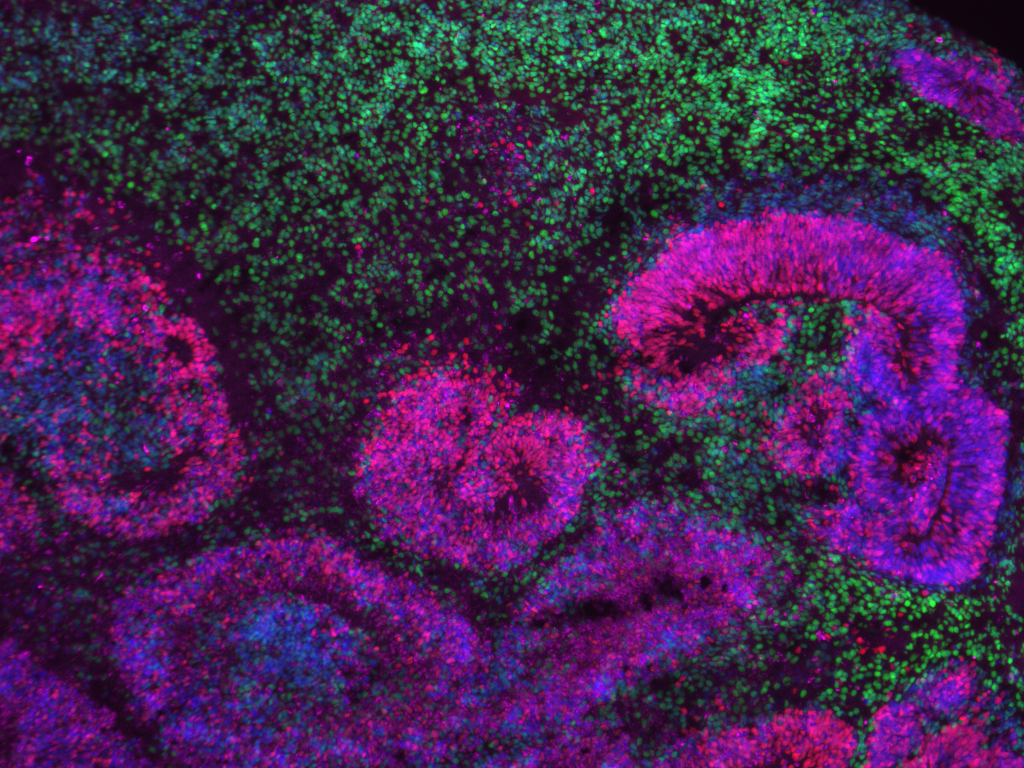
Using patient-derived stem cells carrying the 16p11.2 deletion (a genetic change linked to autism and schizophrenia), we grow mini-brains (“organoids”) and matching “neurovascular” organoids that include blood-vessel cells. We mix-and-match these building blocks, watch them develop in the dish, perform xenograft transplantations into mice, and probe how different diets tweak their growth. Our goal is to pinpoint metabolic and vascular “pressure points” that can be nudged to keep development on course.
CIRM: What are some of the discoveries you’re hoping to achieve through this research project? Can you please tell us about them? What are some research challenges you’d like to overcome through this project?
Dr. Bhaduri: Through this research, we aim to discover:
- Which metabolic pathways set the tempo for early cell-type decisions in the cortex.
- How maturing neurons and blood vessels talk to one another—and how that “neurovascular dialogue” is disrupted by the 16p11.2 deletion.
- Whether specific maternal or post-natal diets can dial disordered development back toward health.
Some of the challenges we’re well-positioned to tackle during this project include:
- Capturing the complexity of human metabolism in a dish.
- Integrating enormous multi-omics and imaging datasets across teams and timepoints.
- Translating findings from organoids and mouse hosts to real-world patients—hence our built-in patient focus groups and clinical co-leads.
CIRM: What are some ways this research project can positively impact patients across California and the world?
Dr. Bhaduri: By revealing metabolic and vascular “switches” that steer brain development, we open the door to new, less-invasive therapies: designer diets, readily delivered small-molecule metabolites, or vascular-targeted drugs that bypass the blood–brain-barrier challenge. Earlier biomarkers gleaned from our data could flag at-risk infants years before symptoms appear, enabling timely interventions and reducing lifelong disability.
CIRM: Can you share why research for neuropsychiatric disorders and diseases affecting the central nervous system is so important?
Dr. Bhaduri: Neuropsychiatric disorders strike one in five people, often in adolescence, and current treatments are blunt and symptom-focused. Understanding the biological roots inside the developing brain is essential to craft precise, side-effect-sparing therapies and close persistent care gaps in underserved communities.
CIRM: The ReMIND program is a pilot for collaborative, multi-investigator funding for foundational basic discovery research. Could you speak to the timeliness and impact of such funding structures more broadly, and why you think such funding structures will be impactful for CIRM’s mission?
Dr. Bhaduri: Cutting-edge questions—like how blood vessels choreograph brain wiring—demand multidisciplinary teams, flexible pilot funding, and fast data-sharing pipelines. The ReMIND program embodies that spirit, allowing metabolism experts, vascular biologists, neurologists, and patient advocates to iterate in real-time. Such structures accelerate basic discoveries into translational pipelines—exactly the mission CIRM was founded to serve.
CIRM: CIRM is celebrating its 20-year anniversary this year. In your words, can you describe CIRM’s impact over the last 20 years?
Dr. Bhaduri: Over two decades, CIRM has transformed California into a global stem-cell powerhouse—from seeding the first human iPSC banks and training thousands of young scientists to shepherding more than 100 clinical trials and pioneering programs like Bridges, which has brought community-college students into labs like ours across California.
Our own team members’ collaboration with specific community colleges—remote organoid projects that put state-of-the-art science into students’ hands—exist because of CIRM’s vision. The agency’s blend of discovery, translational, and workforce funding is a blueprint for how public investment can rewrite the future of medicine.
Learn more about the ReMIND program at cirm.ca.gov/remind.